Aegis Launches: AI Revenue Recovery Engine for Healthcare Providers
"More Appeals. Faster Results. Real Revenue."
💥 TL;DR: Aegis automates the insurance appeals process end-to-end: from denial detection and compliant appeal generation to submission, tracking, and actionable analytics. They integrate with EHRs, clearinghouses, and payer portals, helping providers and medical billing firms recover lost revenue and save significant staff time.
Founded by Krishang Todi, Dhanya Shah & Aarav Bajaj
A team of three close friends from Carnegie Mellon University with deep, complementary expertise across AI, finance, and full-stack development- built for solving complex problems like healthcare claims. Aarav (CS + ML) brings AI research experience and worked at Palantir, where he helped deploy data-driven solutions at scale. Krishang (Econ + Math) did fixed-income risk modeling at one of India’s top funds. Dhanya (IS + CS) is a seasoned full-stack engineer who’s built production systems at three companies. Together, they are building Aegis to bring automation, intelligence, and trust to healthcare appeals.
🩺 The Problem
US healthcare providers lose $260B+ annually to denied claims, and spend $20B+ fighting them. Yet fewer than 15% of denials are appealed - even though over 50% of appeals are successful. With AI-driven denials on the rise, the system is collapsing under its own weight.
The current process of fighting a denial is manual, time-consuming and riddled with inefficiencies.
🧠 The Solution
Aegis plugs into a provider’s existing data stack (EHR, PMS, clearinghouses) to:
- Detect denials automatically: Aegis continuously monitors claims data streams from your clearinghouse and instantly flags denied claims without requiring manual intervention. These denied claims are then arranged by priority based on deadline and claim value.
- Pull patient records, EOBs, and payor docs: Aegis integrates with the EHR to fetch supporting materials, such as patient records, Explanation of Benefits (EOBs), and payer correspondence.
- Generate and submit appeal packages: Using AI trained on successful appeal language and payer requirements, Aegis drafts customized appeal letters, compiles required documentation, and submits the appeal directly to the insurance provider via appropriate channels (fax, portal, or clearinghouse).
- Track appeal progress and surface denial insights: Aegis provides end-to-end tracking of every appeal, including submission confirmation, status updates, and final resolution. Over time, it also analyzes patterns in denials- by payer, procedure, provider, and code- to help providers take proactive steps to reduce future denial rates.

They cut the cost of appealing a denial by 80% and reduce the time to file an appeal from 2+ hours to under 2 minutes.

Learn More
🌐 Visit aegishealth.us to learn more.
🤝 Connect them to: CFOs at hospitals / MSOs, healthcare leaders open to advising, independent practice owners, founders who’ve sold into the RCM stack
✉️ Please shoot the founders an email here.
👣 Follow Aegis on LinkedIn.
Simplify Startup Finances Today
Take the stress out of bookkeeping, taxes, and tax credits with Fondo’s all-in-one accounting platform built for startups. Start saving time and money with our expert-backed solutions.
Get Started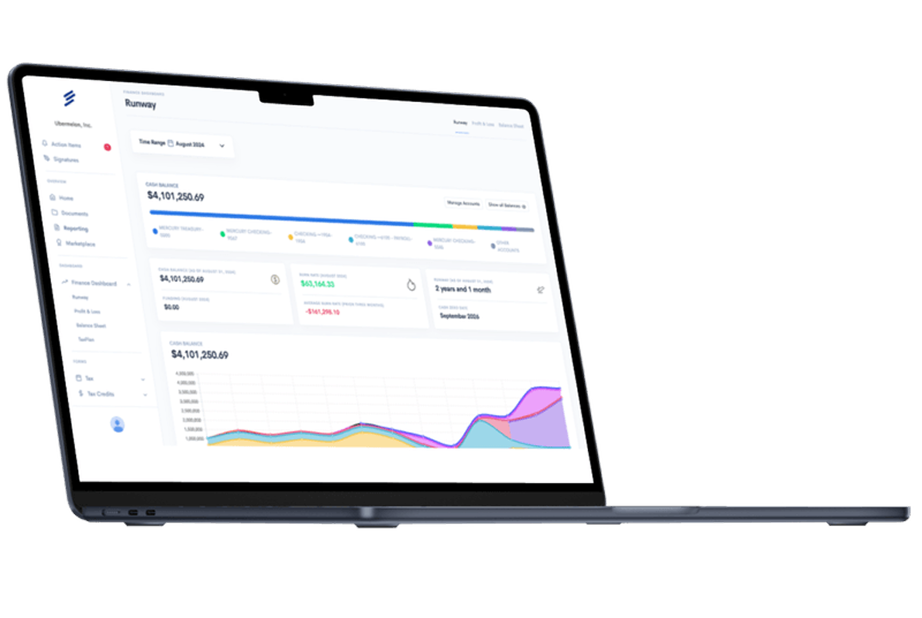









.png)









